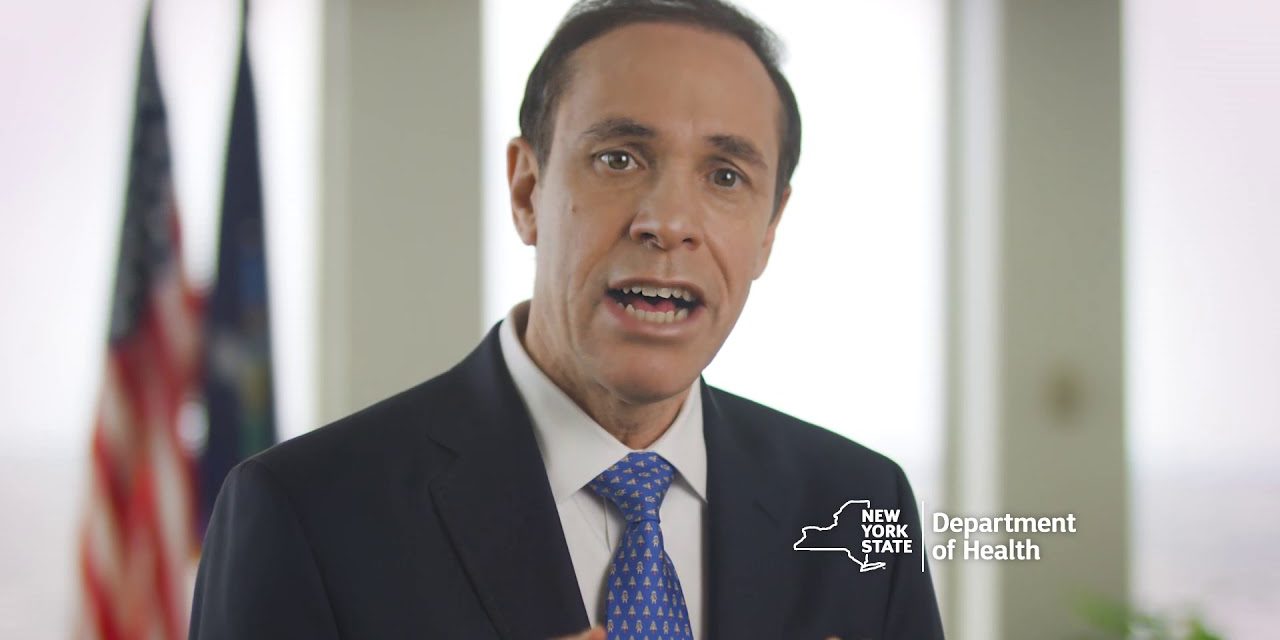
In response to N.Y. Attorney General Letitia James’ 76-page report outlining how the New York State Department of Health may have undercounted nursing home deaths, State Health Commissioner Dr. Howard Zucker released the following statement Thursday afternoon.
The New York State Office of the Attorney General report is clear that there was no undercount of the total death toll from this once-in-a-century pandemic. The OAG affirms that the total number of deaths in hospitals and nursing homes is full and accurate. New York State Department of Health has always publicly reported the number of fatalities within hospitals irrespective of the residence of the patient, and separately reported the number of fatalities within nursing home facilities and has been clear about the nature of that reporting.
Indeed, the OAG acknowledges in a footnote on page 71 that DOH was always clear that the data on its website pertains to in-facility fatalities and does not include deaths outside of a facility. The word “undercount” implies there are more total fatalities than have been reported; this is factually wrong. In fact, the OAG report itself repudiates the suggestion that there was any “undercount” of the total death number.
The OAG’s report is only referring to the count of people who were in nursing homes but transferred to hospitals and later died. The OAG suggests that all should be counted as nursing home deaths and not hospital deaths even though they died in hospitals. That does not in any way change the total count of deaths but is instead a question of allocating the number of deaths between hospitals and nursing homes.
DOH has consistently made clear that our numbers are reported based on the place of death. DOH does not disagree that the number of people transferred from a nursing home to a hospital is an important data point, and is in the midst of auditing this data from nursing homes. As the OAG report states, reporting from nursing homes is inconsistent and often inaccurate.
The Attorney General’s initial findings of wrongdoing by certain nursing home operators are reprehensible and this is exactly why we asked the Attorney General to undertake this investigation in the first place. To that end, DOH continues to follow up on all allegations of misconduct by operators and is actively working in partnership with the OAG to enforce the law accordingly. (pgs 17-21)
The report’s findings that nursing home operators failed to comply with the State’s infection control protocols are consistent with DOH’s own investigation. The report found that operators failed to properly isolate COVID-positive residents; failed to adequately screen or test employees; forced sick staff to continue working and caring for residents; failed to train employees in infection control protocols; and failed to obtain, fit, and train caregivers with PPE. These failures are in direct violation of Public Health Law and DOH guidance that every nursing home operator was aware of. Violations of these protocols is inexcusable and operators will be held accountable. In fact, DOH has already issued 140 infection control citations and more than a dozen immediate jeopardy citations.
The report also found operators in direct violation of the Executive Order requiring nursing homes to communicate with family members in real time when there was a COVID-19 infection or death in the facility. (pg 36)
Additionally, it identifies examples in which nursing home operators reported different information to DOH then to the OAG. To the extent the OAG has identified situations in which nursing home operators submitted false information to the State, the OAG should communicate those discrepancies to DOH so that we can pursue enforcement actions for violations of the Public Health Law. (pg 11) Nursing home operators must report accurate information to DOH or face civil or criminal penalties, and to date DOH has already fined numerous facilities for violating that obligation.
The Attorney General’s report also affirms that the State’s actions to mandate increased testing of nursing home patients and staff, dramatically ramp up testing capacity, provide DOH staff to facilitate testing, and help backfill staffing shortages with the State’s staffing portal directly contributed to a reduction in transmission rates within facilities. (pg 35)
It also affirmed that the State Department of Health’s March 25 advisory memo was consistent with federal CMS and CDC guidance, and in fact was helpful in communities where hospitals had bed shortages during the initial surge. Additionally, the OAG report found no evidence that any nursing home lacked the ability to care for patients admitted from hospitals. (pg 37; page 72, footnote 45)
The OAG report also affirmed the fact that DOH’s March 25 memo was not a directive that nursing homes accept COVID patients from hospitals even if they couldn’t care for them:
‘While some commentators have suggested DOH’s March 25 guidance was a directive that nursing homes accept COVID-19 patients even if they could not care appropriately for them, such an interpretation would violate statutes and regulations that place obligations on nursing homes to care for residents. For example, New York law requires a nursing home to “accept and retain only those residents for whom it can provide adequate care.” See 10 NYCRR § 415.26(i)(1)(ii). Preliminary findings show a number of nursing homes implemented the March 25 guidance with understanding of this fundamental assessment.’ (Pg. 72, footnote 45)
The OAG report also found no evidence that DOH’s March 25 advisory memo resulted in additional fatalities in nursing homes. In fact, a DOH report, which the OAG cites in its own review, found that 98 percent of nursing homes already had COVID in their facilities prior to a patient being admitted there from a hospital. (Page 34 of the DOH report) To quote:
‘The previously reported statewide nursing home survey conducted by NYSDOH on admission data from March 25, 2020 – May 8, 2020 showed that approximately 6,326 COVID-19 patients were admitted from a hospital to a total of 310 unique nursing homes. The updated data now shows that of the 310 nursing homes that took in the 6,326 patients, 304 — or 98% — already had COVID present in the facility prior to admission of a single COVID positive patient from a hospital. In all 304 nursing homes there was at least one suspected or confirmed COVID-positive resident, COVID-related confirmed or presumed fatality, or a worker infected prior to admission of a single COVID-positive hospital patient. Therefore, in these cases, the patient admitted from the hospital did not introduce COVID-19 into the nursing home.’
DOH has consistently found numerous inaccuracies when examining unverified data, and as a result, months ago DOH began an audit of fatality numbers reported by nursing homes to ensure public release of these statistics were accurate. This audit found entries where a deceased individual was listed as dying both in a hospital and in a nursing home, duplicate entries, and entries where the individual had no name or listed a date of death in a facility before they had been admitted, and other issues that suggested inaccurate data inputs. Over the past months, DOH contacted numerous individual facilities to resolve these discrepancies.
DOH has stated on numerous occasions that data will be released once this audit has been completed. Although the audit remains ongoing, DOH data audited to date shows that from March 1, 2020 to January 19, 2021 9,786 confirmed fatalities have been associated with Skilled Nursing Facility residents, including 5,957 fatalities within nursing facilities, and 3,829 within a hospital. This represents 28% of New York’s 34,742 confirmed fatalities — below the national average. Nationally, the Kaiser Family Foundation lists 146,888 nursing home fatalities, 35% of the 423,519 total fatalities reported by the CDC in the United States to date. When 2,957 presumed COVID nursing home fatalities – those fatalities that occurred when testing was scarce and lack confirmed evidence the deceased had COVID – are included, the state’s share of fatalities of individuals that died in nursing homes or in hospitals after transfer is 29.8% of the total number of confirmed and presumed deaths in New York State listed by CDC. For context, states with many fewer total deaths had a similar number of nursing home related deaths, including: Pennsylvania with 10,287 nursing home deaths (49% of their total deaths), Florida with 9,273 nursing home deaths (35% of their total deaths), Massachusetts with 7,944 nursing home deaths (56% of their total deaths) and New Jersey with 7,733 nursing home deaths (36% of their total deaths).
It is worth noting that there remain 13 states that report no information on nursing home fatalities and only nine states, including New York, report nursing home fatalities that are ‘presumed’ COVID and not confirmed COVID. Notwithstanding all of this, the confirmed number of New York State deaths remains unchanged 34,742, and New York’s public COVID dashboard continues to clearly specify that “this data captures COVID-19 confirmed and COVID-19 presumed deaths within nursing homes and adult care facilities. This data does not reflect COVID-19 confirmed or COVID-19 presumed positive deaths that occurred outside of the facility.”
Ultimately, the OAG’s report demonstrates that the recurring problems in nursing homes and by facility operators resulted from a complete abdication by the Trump administration of its duty to manage this pandemic. With no uniform processes or reporting mechanisms, every state reported data in different ways. And data requests from federal CMS, HHS and CDC at various points in the pandemic muddied the reporting across the board. There is no satisfaction in pointing out inaccuracies; every death to this terrible disease is tragic, and New York was hit hardest and earliest of any state as a direct result of the federal government’s negligence. There is still an ongoing crisis that is being actively managed and investigated and we will review the remainder of the recommendations as we continue to fight with every resource and asset to protect all New Yorkers from the scourge of COVID.
All of this confirms that many nursing home operators made grave mistakes and were not adequately prepared for this pandemic, and that reforms are needed, which is why we proposed radical reforms to oversight of nursing home facilities in this year’s State Budget. We will do everything in our power to enact those reforms this year. This is still an ongoing crisis and we will continue deploying every resource possible to ensuring the health and safety of every single New Yorker.